November 2, 2024
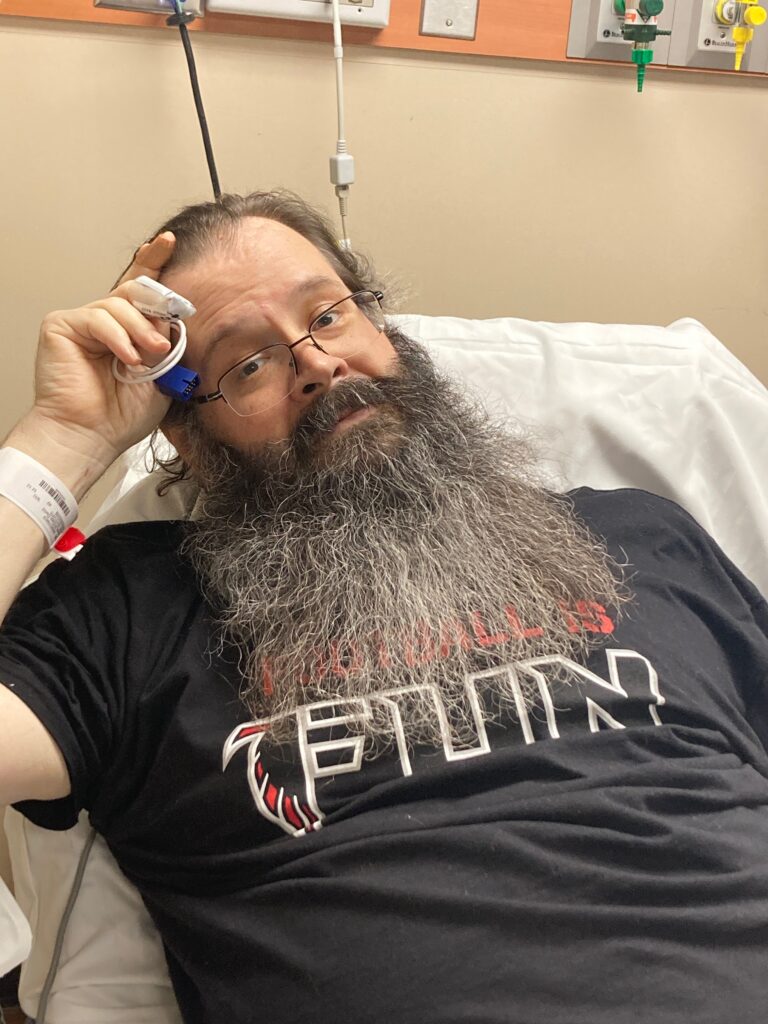
David got up this morning with a temp of 101.7. I gave him some rapid release Tylenol and he took all his other morning meds. Knowing we are supposed to call the oncologist’s office for temps over 100.5, we wanted to see if the Tylenol helped get it down before we called. After about 20 minutes, I noticed him making sounds like he was trying to talk. I asked him what he was feeling, and he was noticeably having issues making a complete sentence or thought. He expressed he was aware that he was having difficulty finding the words and there were long pauses in his speech. He never slurred and when I asked, he could tell me things like who he was, the date, who the president was, etc. I took his temp again and it had risen to 102.9. I called the oncologist’s office and waited on the doctor on call to phone us back. We got the call in about 10 minutes and after I explained what David was experiencing he asked how close the nearest hospital was to us. I told him about 10 miles and he said go on and go and get checked out for an infection. I asked if this meant being admitted because we would prefer to be admitted at a Piedmont Hospital if that was the case. He said he understood but did not want me to drive while he was confused and would be best to get to the local hospital for eval and then we could decide. He said they could call in and he would talk to them. David wanted to shower first so he took a cool shower and I packed a few things he may need since we didn’t know how long we would be gone. By the time we were leaving, he had more control over his speech and felt better. When we left home, his temp was 99.7. We headed out and got to URMC around 10:45 this morning. They triaged him and he went right for which we are very grateful. His BP was normal and heart rate was normal for him (it runs high) and his temp was 99 at that time. They asked tons of intake questions and assessed him for stroke or TIA due to the earlier confusion. A call was made to get him back to the ER and go for chest Xray and head CT to start ruling things out. Radiology came for him right away and he was gone about 15 minutes while I waited in the little room. Once he was back, the lab was there to take blood and one of the nurses got a bag of fluid going. The ER doctor came in to discuss what he was feeling and asked about the cancer and treatments. I rattled off the chemo meds he had this week and the doctor said he was impressed. He said they didn’t always get that level of info. I thought if he only saw all the notes I take. I guess I feel like it is my job because I cannot do anything else and feel useless if I can’t do something. I gave him a copy of the treatment orders, so he had all the dosages and phone number for Dr. B’s office. The lab came back to take more blood for a culture and also asked for a urine sample. All blood work came back normal even his WBC, which they thought may possibly be low, was also within range. His glucose was high (219) but with the morning like it was, he didn’t a proper breakfast so was unable to take that medication prior to his meal. The culture would take 24 hours or so and the ER doctor discussed admitting him to monitor while we are waiting to see if there is sepsis. We asked that he call the Oncologist and discuss with him first. The Onc on call said since there was no clear indication of a source of infection and David looked and felt ok , that he could go home without antibiotics and we could monitor his temp using Tylenol and Advil alternately to control any fever. The ER doctor advised that we were to come straight back if the temp rose high again and especially if there were accompanying symptoms such as the confusion. He said they cultures were flagged and we would get a call if something showed up in them that warranted treatment. We waited a forever amount of time for the paperwork to go home and left around 4:20. His temp when we left was around 99 so it had stayed there without medication. David said he felt ok but was just ready to get home. Once home, he had some soup and tried to relax on the couch. He said he couldn’t get relaxed and felt agitated. He took his evening meds after he ate and started to settle down a little. I took his temp a few times and it was 100.1 around 6pm and then after Tylenol, it has hovered around 98. He got really sleepy and slept a while on the couch while I updated the notes from today and started reading something I began a few days ago about Serotonin Syndrome. This sounds a lot like what may be happening since he takes medications that interact with each other and each creates additional serotonin. I don’t know if it is anything but the symptoms tracked for what he has been experiencing today. I plan to bring it up to Dr. B or maybe Dr. W here in town on Monday. The hospital advised following up with Dr. W in 2 days anyway. It could also just be chemo fever that occurs following an aggressive chemo treatment. Been reading up on that too. Hoping for a better night and morning than we had today. Grateful for being home and that we feel we received good care today. I am starting to feel wiped out now. It is amazing how long your body holds on to adrenaline when you have to kick into action. Why does time stand still in a hospital though?